Having a stabbing ache in your lower belly or a bloated, heavy sensation that time won’t wash away? It may be a paraovarian cyst.
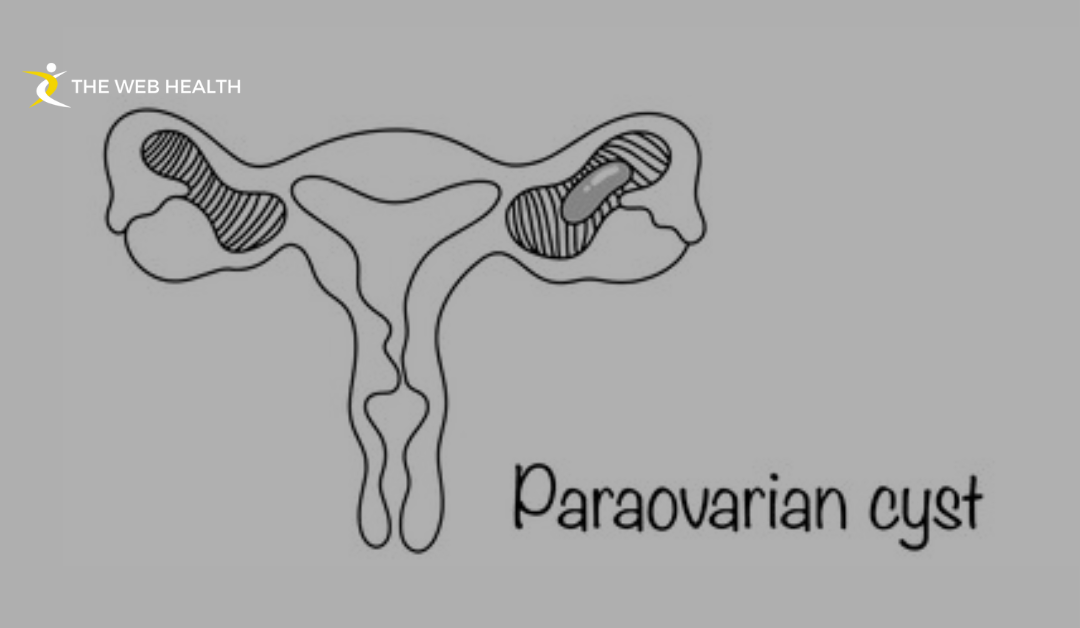
Paraovarian cysts, which are located beside the ovary near the fallopian tubes, grow outside the ovary, unlike ovarian cysts. These cysts represent 5%–20% of adnexal masses and are usually unrecognized unless they are large enough to cause discomfort. Rare complications, such as torsion or rupture, may also develop.
Should you be concerned? Can they impact fertility or need surgery? Read on — this guide tells you everything you need to know!
What Is a Paraovarian Cyst?
Paraovarian cysts are fluid-filled sacs forming close to the ovary or the fallopian tube. Unlike ovarian cysts, which occur on the inside of the ovary, paraovarian cysts form in the broad ligament — the tissue that attaches the uterus to the ovaries and fallopian tubes.
Doctors may refer to them as paratubal cysts or cysts of Morgagni.
These cysts are often small and don’t connect to the ovary itself. They are derived from remnants of embryonic structures known as Müllerian and Wolffian ducts. Due to their location, they typically go unnoticed unless they grow larger or cause symptoms.
Causes of Paraovarian Cysts
Doctors don’t know exactly what causes paraovarian cysts to form, but some common causes are:
- Remnants of Embryonic Tissue – These cysts generally arise from residual tissue of the Müllerian and Wolffian ducts formed during fetal development.
- Hormonal Imbalances – Changes in estrogen and progesterone can promote the growth of cysts.
- Genetics – The risk may be greater if family members have had ovarian or paraovarian cysts.
- Peritoneal Inclusion Cysts – In some cases, fluid trapped in the pelvic area can form cysts.
- Lifestyle Factors – Although not directly related, bad eating habits, high levels of stress and some medications can promote hormone-related cysts.
How Can You Tell If You Have a Paraovarian Cyst?
Many paraovarian cysts do not cause noticeable symptoms and are only found during routine pelvic exams or ultrasounds. However, larger cysts may lead to:
- Pelvic Pain or Discomfort: This can be a dull ache or sharp pain, often felt on one side of the lower abdomen. Some women find relief through therapies like pelvic floor therapy, which helps strengthen pelvic muscles and improve overall comfort.
- Abdominal Bloating or Fullness: A feeling of heaviness or swelling in the lower abdomen.
- Frequent Urination or Bowel Changes: Large cysts may press against the bladder or intestines, causing changes in bathroom habits.
- Irregular Menstrual Cycles: Some women notice changes in their period flow or timing.
- Fatigue or Weakness: If the cyst causes internal bleeding, it may contribute to low iron levels, leading to tiredness and dizziness.
When to Worry
Get medical attention immediately if you have:
- Severe, sudden pain – This could mean the cyst has ruptured.
- Nausea or vomiting – A sign of ovarian torsion (twisting).
- Heavy bleeding – Rare but possible with ruptured cysts.
Diagnosing a Paraovarian Cyst
There are multiple ways through which doctors detect a paraovarian cyst. Because most cysts don’t produce symptoms, they are commonly discovered incidentally during routine checkups or imaging tests. If you have pelvic pain or unusual bloating, your doctor might do specific exams to confirm the cause.
1. Pelvic Exam
Diagnosis typically begins with a pelvic exam. The doctor gently presses on the lower abdomen to check for any lumps or swelling. While small cysts may be too deep to detect manually, larger cysts, especially those over 5 cm, can sometimes be felt as a soft, movable mass near the ovary.
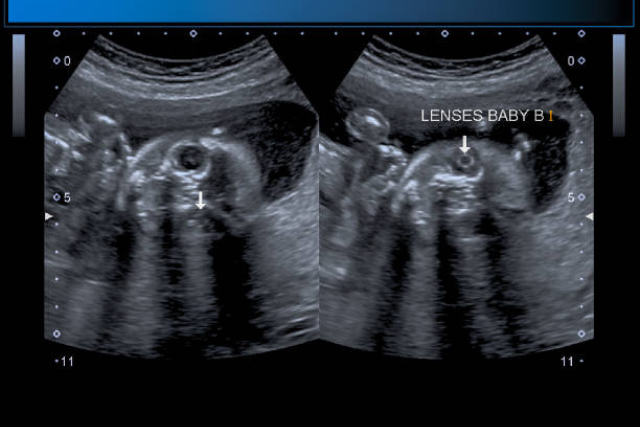
2. Paraovarian Cyst Ultrasound
The most common test used to diagnose a paraovarian cyst is ultrasound. It uses sound waves to produce images of the reproductive organs.
- What Ultrasound Shows – The scan helps determine the size, shape, and location of the cyst.
- Simple vs. Complex Cysts – A simple cyst contains clear fluid and is typically harmless. A complex cyst has solid portions or thick walls, which may require additional testing.
Doctors can use two types of ultrasound:
- Transabdominal Ultrasound – A probe is placed on the lower belly to view the cyst.
- Transvaginal Ultrasound – A small probe is inserted into the vagina for a clearer image of smaller cysts.
3. MRI or a CT Scan
An ultrasound is usually sufficient to diagnose a paraovarian cyst. If the cyst appears atypical or has complex characteristics, though, doctors may order extra imaging:
- MRI (Magnetic Resonance Imaging) – Provides a detailed view of soft tissues and can help differentiate a benign cyst from something more serious.
- CT Scan (Computed Tomography) – Sometimes applied when the cyst is too large or suspected to push on nearby organs.
ICD-10 Code for Paraovarian Cyst
For medical documentation, the ICD-10 code N83.2 is used for paraovarian cysts. This code helps with tracking diagnoses, processing insurance claims, and planning treatment.
Are Paraovarian Cysts Harmful? When Should You Worry?
These cysts are almost always benign (non-cancerous) and remain unnoticed for years. But at times, they can cause complications that require a medical intervention.
1. Cyst Rupture
A paraovarian cyst may rupture when it is too large or subjected to sudden pressure. If this occurs, symptoms might include:
- Sharp, sudden pain in the lower abdomen
- Nausea or vomiting
- Internal bleeding (if a blood vessel is affected)
Severe pain that does not subside requires immediate medical attention.
2. Ovarian Torsion (Twisting of Fallopian Tubes)
A big cyst can push the ovary or fallopian tube out of position. This twisting, or torsion, cuts off blood flow and results in:
- Severe, crampy abdominal pain
- Nausea or fever
- Dizziness or fainting
Torsion is an emergency. Seek medical help immediately if these symptoms appear.
3. Risk of Malignancy (Rare, But Possible)
There are many paraovarian cysts that are benign. But rarely some grow abnormally. Warning signs include:
- Rapidly increasing size
- Solid areas visible on an ultrasound
- Unexplained weight loss
Doctors may order additional tests, such as an MRI or a biopsy, to exclude the possibility of cancer.
When Should You Be Concerned About Cysts?
Treatment for small cysts is typically not necessary. Doctors may also recommend removal of a cyst larger than 5 cm to avert rupture or torsion. The surgery is most often minimally invasive (laparoscopy) with a short recovery period.
Can You Get Pregnant with a Paraovarian Cyst?
Most women who have paraovarian cysts can get pregnant naturally. These are formed outside the ovary, so they don’t interfere with either egg production or implantation. A small cyst generally remains benign. If it becomes large, it can put pressure on the fallopian tubes, which makes conception more difficult.
Do Pregnancy Hormones Cause the Cyst to Grow?
Estrogen and progesterone increase during pregnancy, which might cause some cysts to grow. Many of them stay small, and trouble-free. But if one grows rapidly, it may cause pain or pressure in the lower abdomen.
Should a Doctor Remove the Cyst Before Pregnancy?
They may need to be surgically removed if:
- The cyst is larger than 5 cm and there is a risk of torsion (twisting) or rupture.
- It results in persistent pain or pelvic pressure.
- The doctor thinks it may be abnormal or cancerous growth.
Minimally invasive surgery, such as laparoscopy, is often used to remove cysts while preserving reproductive health.
Risks of a Paraovarian Cyst in Pregnancy
Most women who harbor these cysts are able to carry their pregnancies without complication. Still, some risks exist:
- Cyst Torsion (Twisting): A large cyst may twist around its blood supply, cutting circulation to the ovary or fallopian tube. This can cause sharp pain and may require emergency surgery.
- Pressure on the Uterus: A growing cyst might push against the uterus, creating discomfort or affecting the baby’s position.
- Effect on Delivery: Small cysts rarely interfere with labor. A larger one might block the birth canal, making a C-section necessary.
Women with paraovarian cysts should get regular checkups to ensure a smooth pregnancy and safe delivery.
Treatment Options for Paraovarian Cysts
As mentioned before they are usually harmless and do not always require treatment. The best approach depends on the size of the cyst, symptoms, and potential risks.
When Doing Nothing Is the Best Option
If a cyst is small (less than 5 cm) and not causing symptoms, doctors may recommend a wait-and-watch approach. This means:
- Regular ultrasound scans to monitor changes in size.
- Checking for new symptoms like pain, bloating, or pressure.
- No immediate treatment unless the cyst grows or causes discomfort.
For many women, small paraovarian cysts stay the same size or even disappear on their own. However, persistent discomfort, much like recurring foot pain, should not be ignored, as it might indicate an underlying issue requiring medical attention.
Medical Monitoring
Your doctor may suggest frequent follow-ups if:
- The cyst is growing but still under 5 cm.
- It has an irregular shape or unusual fluid content.
- There is mild discomfort but no urgent need for surgery.
Regular ultrasounds (every 6 to 12 months) help track any changes.
Surgical Removal (Paraovarian Cystectomy)
If a paraovarian cyst grows larger than 5 cm, causes severe pain, or shows suspicious signs, surgery may be necessary.
Laparoscopic vs. Open Surgery
- Laparoscopic Surgery (Minimally Invasive)
- Best for cysts under 10 cm with no signs of cancer.
- Small incisions, less pain, and faster recovery.
- Outpatient procedure (most women go home the same day).
- Open Surgery (Laparotomy)
- Used for very large or complex cysts.
- Requires a larger incision and longer recovery.
- Necessary if there is a concern about malignancy.
When Surgery Is Recommended
Doctors suggest removal if:
- The cyst keeps growing or exceeds 5-7 cm.
- You experience severe pain or pressure.
- The cyst twists (torsion) or ruptures.
- There is suspicion of cancer (rare but possible).
Alternative Treatments
While diet and lifestyle changes cannot remove a paraovarian cyst, they may help reduce inflammation and support hormone balance. Some tips include:
- Eating anti-inflammatory foods (leafy greens, berries, nuts, fish).
- Limiting processed foods and sugar, which may contribute to hormonal imbalances.
- Staying active to promote overall reproductive health.
However, there is no scientific evidence that diet alone can shrink a paraovarian cyst. Always follow your doctor’s advice.
Prevention and Long-Term Management
There is no guaranteed way to prevent paraovarian cysts because they often develop from embryonic tissue. However, certain habits may lower your risk of developing large or problematic cysts.
Lifestyle Factors That May Reduce Risk
- Maintaining a healthy weight: Obesity is linked to hormonal imbalances.
- Balancing hormones naturally: Reducing stress, getting enough sleep, and avoiding endocrine disruptors (like BPA in plastics) may help.
- Avoiding unnecessary hormone treatments: Some medications can increase cyst development. Always discuss risks with your doctor.
The Role of Regular Gynecological Checkups
Regular visits to a gynecologist are essential for detecting cysts early. Doctors may recommend:
- Annual pelvic exams to check for abnormalities.
- Ultrasounds if you have symptoms or a history of cysts.
- Early intervention if a cyst shows signs of growth or complications.
FAQs About Paraovarian Cysts
Can paraovarian cysts go away on their own?
Yes, small paraovarian cysts (less than 5 cm) can often resolve without treatment. Most cysts are harmless and do not change, and so do not cause any symptoms. But ongoing monitoring is important to make sure they don’t get bigger or lead to complications.
What size paraovarian cyst necessitates surgery?
Cysts larger than 5–7 cm usually need surgery, particularly if they cause pain, pressure, or complications such as torsion or rupture. Small cysts that don’t grow or cause symptoms are usually monitored rather than surgically removed.
What happens if a paraovarian cyst bursts?
If a cyst ruptures, it can cause:
- Sudden, sharp pelvic pain
- Internal bleeding (in rare cases)
- Nausea or dizziness
Most ruptured cysts heal on their own, but severe pain or heavy bleeding requires immediate medical attention.
Are paraovarian cysts linked to PCOS?
No, they aren’t connected, because:
- PCOS involves multiple small cysts inside the ovaries, linked to hormone imbalances.
- Paraovarian cysts develop outside the ovary and are not caused by PCOS.
How often should paraovarian cysts be monitored?
For small, non-symptomatic cysts, doctors suggest an ultrasound once every 6 to 12 months. If a cyst grows or causes pain, it may require more regular monitoring or treatment.
Last Words
The majority of paraovarian cysts are harmless and do not require treatment. But if a cyst grows, becomes painful, or has unusual characteristics, medical monitoring or surgery may be necessary. Regular checkups help ensure early detection and peace of mind.