No one wants to hear the word “cancer,” but the truth is there are over 200 types of cancer that exist, and oral cancer is one of them. Although it’s a common form of cancer, it often slips under the radar.
This year, approximately 58,450 Americans received a diagnosis of oral or oropharyngeal cancer. And sadly, it leads to over 12,250 deaths.
One of the biggest challenges is that its symptoms can be subtle—things like stubborn sores or unusual patches—and may be mistaken for something less serious. This can lead to delays in diagnosis.
But early diagnosis is crucial, as it increases survival rates above 80%. Oral cancer is often squamous cell carcinoma and occurs in the mid-sixties.
Knowing the signs, understanding how it differs from gum disease, and taking preventive steps can improve outcomes and save lives.
Now let’s discuss oral cancer in more detail.
What is Oral Cancer?
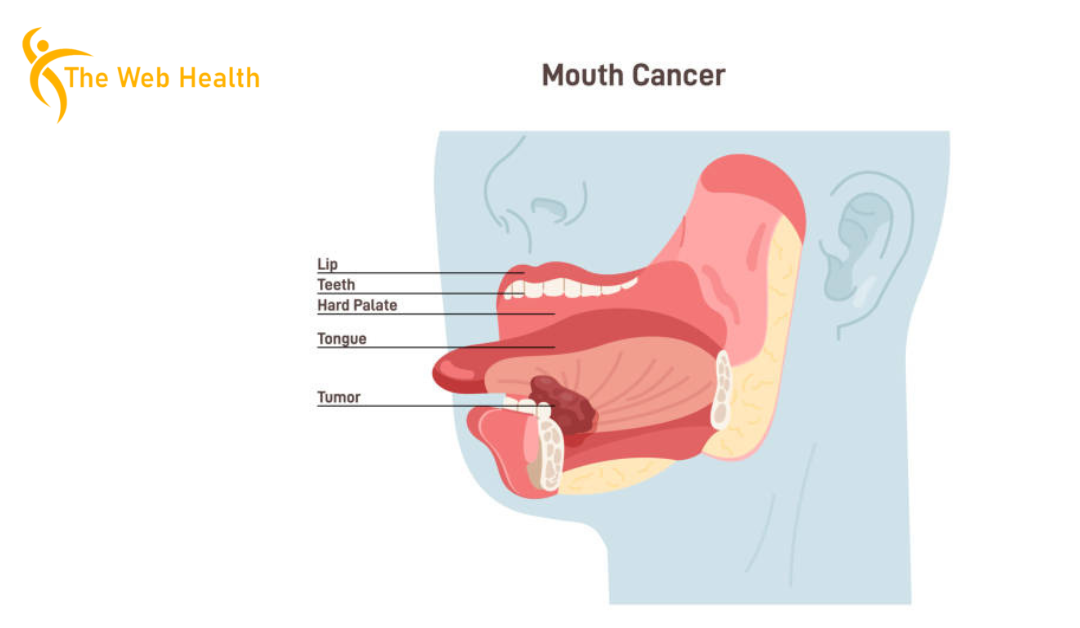
Oral cancer, also known as mouth cancer, refers to cancer that occurs when cells in your mouth or throat grow out of control. It can be split into two types:
- Oral cavity cancer
- Oropharyngeal cancer
Oral cavity cancer affects the parts of the mouth you can see, like the lips, tongue, gums, the floor, and the roof of your mouth.
Oropharyngeal cancer shows up in the back part of your mouth, including the tonsils and the base of the tongue.
Though these cancers have some similar signs and overlap, their treatment and recovery can be different.
Common Areas Affected
Oral cancer can show up in different areas of your mouth, like:
- Lips
- Gums
- Tongue
- Floor of the Mouth
- Roof of the Mouth
Signs and Symptoms
Oral cancer often starts slow, with little warning signs. At first, it might feel like a small problem, but it’s important to stay alert. If you notice something unusual in your mouth, don’t ignore it.
Early Signs to Watch For
Some early signs to look out for include:
- Sores or Ulcers: These might stay for more than two weeks without healing.
- White or Red Patches: These patches may appear on your tongue, gums, or inside your mouth.
- Lumps or Thickening: You might feel a bump inside your cheek, on your gums, or under your tongue.
These signs can be easy to miss, but if they stick around, it’s best to see a doctor.
Advanced Symptoms
If oral cancer is left untreated, it can spread and cause more serious issues. Advanced symptoms might include:
- Difficulty Swallowing or Chewing: You might notice a sore throat that won’t go away or trouble eating certain foods.
- Weight Loss: Unexplained weight loss can happen if cancer starts to affect your body’s ability to eat or absorb nutrients.
- Pain: This could show up in your mouth, ears, or neck.
Remember, these symptoms can also be caused by less serious issues like an infection or inflammation. That’s why early detection is so important. It’s better to get checked out than risk waiting too long.
Oral Cancer vs Gum Disease
Many people confuse oral cancer with gum disease because of the similar symptoms but they are two different conditions with different causes, progression and severity.
Gum disease or periodontal disease is caused by neglect of oral hygiene. Plaque builds up and causes gum irritation, bleeding and potentially tooth loss. Symptoms are swollen gums, bad breath that won’t go away and tenderness. While gum disease can be severe it’s rarely life threatening and can be reversed with good dental care.
Oral cancer is a much more serious condition. It’s unchecked cell growth in areas like tongue, throat or lips. Unlike gum disease, oral cancer can metastasize to other parts of the body if not treated immediately. Persistent sores, unusual lumps or unexplained bleeding are common symptoms of this condition.
Causes and Risk Factors
Knowing what increases your risk of oral cancer helps you make smarter decisions. While prevention is not always possible, being aware of the major risk factors will enable you to take proactive steps.
Tobacco Use
Tobacco is a major contributor to oral cancer. Whether through smoking cigarettes, cigars or using smokeless products the risk is high. Quitting all tobacco habits will lower your risk of oral cancer by a significant amount.
Alcohol Consumption
Excessive alcohol consumption increases the risk. When combined with tobacco use the risk is even higher. Limiting alcohol or eliminating it altogether is a powerful protection against oral cancer.
HPV (Human Papillomavirus)
Some HPV strains are linked to mouth and throat cancers. This sexually transmitted virus can increase your risk. Vaccination against HPV is a powerful protection against future related cancers.
Genetic Predisposition
A family history of cancer including oral cancer increases your inherent risk. Genetics determines how your body reacts to environmental factors. Regular medical checkups and early detection is crucial for those with such predispositions.
Other Risk Factors
- Poor Oral Care: Not taking perfect care of your teeth and gums creates an environment for disease.
- Sun Exposure: Overexposure to the sun, especially on your lips, can lead to cancer. Always wear lip balm with sunscreen when outdoors.
By addressing these factors you can lower your risk of oral cancer but no prevention is 100% guaranteed. Prioritize good oral hygiene, minimize risky habits and consult a doctor are the keys to protecting your health.
Stages of Oral Cancer
Oral cancer has different stages, and understanding them is important for finding the right treatment and boosting survival chances. Doctors use the TNM system to figure out how big the tumor is, if it’s spread to nearby lymph nodes, and whether it has moved to other parts of the body. This helps them decide what treatment will work best.
TNM Staging System and Signs of Oral Cancer
The TNM system is the main way to track how oral cancer progresses. It looks at tumor size, lymph node spread, and if the cancer has reached other organs. Let’s explore the stages and their warning signs:
Understanding TNM Staging
T (Tumor Size)
- T1: The tumor is smaller than 2 cm.
- T2: The tumor ranges from 2 to 4 cm.
- T3: The tumor is larger than 4 cm.
- T4: The tumor spreads to nearby areas like the jaw or tongue.
N (Lymph Nodes)
- N0: No cancer in the lymph nodes.
- N1: Cancer has spread to one lymph node on the same side of the neck.
- N2: Multiple lymph nodes are affected, or nodes are on both sides of the neck.
- N3: Cancer has spread to large lymph nodes.
M (Metastasis)
- M0: Cancer hasn’t spread to other organs.
- M1: Cancer has spread to distant parts of the body.
Stages of Oral Cancer
Oral cancer is grouped into four stages:
Stage I: The tumor is small and has not spread to lymph nodes or other areas. This stage has the best survival rate.
Stage II: The tumor is bigger than Stage I but hasn’t spread.
Stage III: The tumor may have spread to lymph nodes but not to distant organs. It might also be bigger.
Stage IV: Cancer has spread to distant organs and is usually harder to treat. The size of the tumor may also be larger.
Symptoms at Different Stages
Pre-cancerous and Stage I Symptoms:
In the early stages, oral cancer might not hurt. However, some signs to watch for include:
- White patches (leukoplakia) that might be pre-cancerous.
- Red patches (erythroplakia) that could signal danger.
- A mix of red and white patches (erythroleukoplakia).
- Sores or ulcers that don’t heal after two weeks.
- Thickening of the inside of the mouth.
Look inside your mouth often for these signs. If something looks odd and doesn’t go away, see a doctor.
Stage II and III Symptoms:
As the tumor grows, it may affect nerves and muscles, causing:
- Numbness or loss of feeling around the mouth, jaw, or tongue.
- Pain or discomfort that gets worse.
- Swollen lymph nodes in the neck or jaw.
- Difficulty chewing or speaking.
- Dentures that don’t fit properly.
If you notice these changes, it’s important to see a doctor quickly.
Stage IV Symptoms:
At this advanced stage, cancer can spread to other parts of the body, causing severe symptoms like:
- Trismus (lockjaw), where you can’t open your mouth fully.
- Loose teeth or changes in how teeth fit together.
- Swelling in the jaw or tongue.
- Lumps in the neck as cancer spreads to lymph nodes.
- Weight loss and fatigue if the cancer has spread to distant organs.
Stage IV oral cancer requires urgent and complex treatment. It can also affect other parts of the head and neck, making recovery harder.
Other Symptoms of Oral Cancer
Oral cancer can also cause:
- Pain while swallowing.
- Hoarseness or a constant earache.
- Bleeding from an ulcer or sore that doesn’t stop.
Diagnosis and Tests
Early diagnosis of oral cancer is crucial for effective treatment. However, many people are unaware of the signs and often ignore early symptoms. That’s why regular check-ups with a dentist are essential. Dentists are trained to identify any changes in the mouth that might indicate cancer. But if your dentist or doctor suspects oral cancer, they’ll recommend tests to confirm the diagnosis.
Physical Examinations and Self-Checks
The first step in diagnosing oral cancer is a thorough physical exam. Dentists and doctors will look inside your mouth for any unusual signs, such as sores, white or red patches, lumps, or swelling. They’ll also check your neck for any enlarged lymph nodes.
You can also perform a basic self-check at home. Here’s how:
- Look inside your mouth with a mirror. Check the roof, floor, tongue, and inner cheeks for sores or unusual spots.
- Feel the area under your jaw and on the sides of your neck for lumps or swelling.
- Pay attention to any persistent pain, soreness, or difficulty swallowing. If these issues last longer than two weeks, make an appointment with your dentist or doctor.
If something seems unusual, don’t wait for a check-up. Early detection increases the chances of a successful treatment plan.
Diagnostic Procedures
Once your doctor or dentist identifies something of interest, then more tests are required. The following procedures can help confirm a diagnosis:
- Brush Biopsy: A brush biopsy is not invasive. Your doctor employs a brush that is specially designed to scrape cells from the area of concern. These cells are then send to the laboratory for testing. This test can be used to detect early signs of cancer without having to go for a more rigorous test.
- Incisional Biopsy: if the brush biopsy does not yield a diagnosis, an incisional biopsy may be performed. This will involve taking a biopsy of the affected area by taking a small piece of tissue and taking it for analysis. If the lesion is larger or deeper an incisional biopsy is usually performed.
- Imaging Techniques: If the doctor thinks that the patient has oral cancer, other imaging tests such as CT scan or MRI may be advised. These tests provide a clear picture about the particular region detailing doctors in case cancer has extent its tendrils to surrounding lymph nodes or to any other organ.
Diagnosis is the first step in the fight against oral cancer. The quicker it’s identified, the better the chance for successful treatment. If you notice any changes in your mouth or experience unexplained symptoms, don’t hesitate to get checked. Early action can save lives.
Treatment Options
The treatment plan for oral cancer is quite different in each case, depending on the specifics of the case. Surgery is one of the most common treatments for oral cancer, although there are several methods employed in the treatment process. The treatment of cancer is not a one size fits all approach and can include surgery, radiation therapy, chemotherapy or a combination of the three.
Surgery: Types and What to Expect
Surgery is the most preferred treatment method in oral cancer. It is to excise the tumor and the adjacent tissue which contains cancer cells. The kind of surgery to be done depends on the size, location and stage of the cancer.
- Tumor Removal: In the case of small tumors, a surgeon may only have to excise the tumor. It could be a simple procedure.
- Reconstructive Surgery: Sometimes cancer affects large parts of the mouth or jaw. In this case, doctors may need to rebuild the area. They might take tissue from somewhere else in your body, like the arm or thigh, and use it to fix the affected area. This helps restore function and look.
- Neck Dissection: If the cancer spreads to the lymph nodes in the neck, doctors may do a neck dissection. This procedure removes lymph nodes to stop cancer from spreading. It might be done with other treatments like radiation.
Radiation Therapy and Its Applications
Radiation therapy uses high-energy rays to kill cancer cells. It is useful when surgery cannot remove the tumor or isn’t an option. Radiation is also helpful after surgery to kill any remaining cancer cells, lowering the chances of the cancer returning.
Radiation may be done from outside the body. A machine directs rays to the affected area. Or, doctors may use brachytherapy, which places radioactive material inside the mouth near the tumor.
Side effects include sore throat, mouth, and trouble swallowing. You may also have dry mouth or changes in taste. These effects often go away but can be controlled with care.
Chemotherapy and Immunotherapy
Chemotherapy uses strong drugs to kill or slow the growth of cancer cells. It’s used when cancer spreads to other parts of the body or when surgery and radiation are not enough. Chemotherapy can be taken as pills, shots, or through an IV.
Even though chemotherapy kills cancer, it also harms healthy cells. This causes side effects like nausea, hair loss, and weakness. Doctors may change the plan to make it easier on the body.
Immunotherapy helps the body fight cancer by boosting the immune system. This treatment is newer and may work when other treatments fail. Immunotherapy has shown good results in fighting advanced oral cancers, though it is still being tested.
Emerging Treatments and Holistic Approaches
Scientists are working on new ways to treat oral cancer. One treatment is targeted therapy. This method uses drugs to attack cancer cells without harming healthy ones. Another method, gene therapy, works by fixing the gene problems that cause cancer.
Some people also try holistic treatments. These include acupuncture, herbal medicine, or changing their diet. These treatments won’t cure cancer, but they may help ease side effects or improve health. Always talk to your doctor before trying anything new.
Oral Cancer Survival Rates & Prognosis
Oral cancer prognosis is determined by the stage at which the cancer is diagnosed, the patient’s age and general health, and the cancer’s sensitivity to treatment. These details make it possible to predict what might happen in the future.
Survival Rates by Stage
The probability of living after oral cancer is much higher when the doctors diagnose it at an early stage. According to the American Cancer Society, the five-year survival rate of oral cancer patients whose cancer is confined to the oral cavity is 84%. But, if the tumor is in the lymph nodes or other parts, the survival rate is low.
- Stage I: If the cancer is localized to a small area of the mouth, the chances of survival are 80-90%. Fortunately, most of those who are diagnosed early can be cured completely.
- Stage II: At this time, cancer might have spread to the adjacent tissues or liver and /or nodes. The survival rate reduces to 60-80 percent depending on the stage that the cancer has reached.
- Stage III: Cancer has reached other lymph nodes or tissues near the mouth. The survival rate is between 40-60%.
- Stage IV: In case the cancer metastasizes to other parts of the body, the survival rate drops below 40%. In this stage, both the treatment and prognosis can be centered on pain relief and comfort.
What Affects Survival Rates?
A few things can affect how well a person does after an oral cancer diagnosis:
- Age and Health: The young and the healthy are usually quick to recover from the sickness. Patients with other diseases or of older age may experience more problems with treatment.
- Early Detection: The more early the cancer is detected, the higher the possibility of it being treated. In order to diagnose the disease the patient needs to have routine check-ups with a dentist and also self-exam every mouth.
- Tumor Location and Size: Cancerous growths that are located in areas that can be easily accessed or have not metastasized yet have better prognosis. If cancer is localized in sensitive areas such as the jaw or throat, then treatment becomes more complicated and risks are increased.
- Response to Treatment: There are some types of cancer that are hard to cure. The effectiveness of the surgery, radiation or chemotherapy may determine the extent of the result.
Prevention of Oral Cancer
While you can’t completely remove the risk of oral cancer, you can take steps to reduce your chances of developing it. Most of these steps focus on daily habits, choices, and keeping up with regular health check-ups. Here’s what you can do to protect yourself.
Avoiding Tobacco and Alcohol
Tobacco use and alcohol consumption are the biggest risk factors for oral cancer. Smoking or chewing tobacco raises your risk significantly, as does drinking alcohol, especially if you combine the two. These habits harm the cells in your mouth and throat, making it easier for cancer to develop.
If you use tobacco, quitting will greatly improve your health. If you drink alcohol, you might want to cut back or quit altogether to lower your risk.
The Significance of HPV Vaccination
HPV is now considered as one of the leading causes of some oral cancers particularly of oropharyngeal origin. HPV associated oral cancers have been increasing and this trend is observed among the young generation. The good news is that there is a vaccine that can prevent some of the types of HPV.
The HPV vaccine is both safe and effective. Doctors recommend it for both boys and girls at age 11 or 12, but it can also be given to people up to 26. Getting vaccinated can lower the chances of developing HPV-related cancers in the mouth and throat.
Regular Check-Ups and Self-Exams
One of the most effective ways of early detection of oral cancer is through a routine visit to your dentist. Dentists are taught to look for signs of cancer in your mouth, throat or any other part of the body. They can detect symptoms before you realize that there is something wrong with you. It is advisable to go for check up at least once a year.
Besides dental visits, you can do self-exams to check for any odd changes in your mouth. Look for sores, white or red patches, lumps, or any pain that doesn’t go away. If you spot anything unusual, don’t wait for your next dentist visit—make an appointment right away.
Healthy Eating for Oral Health
Eating the right foods can also help lower your risk of oral cancer. A healthy diet with plenty of fruits, vegetables, and whole grains can strengthen your immune system and help fight off cancer cells. Foods high in antioxidants may protect your cells from damage.
Try adding berries, leafy greens, carrots, and tomatoes to your meals. These foods are full of nutrients that support your oral health and overall well-being.
Living with Oral Cancer
A diagnosis of oral cancer is life-changing. For both patients and their families, coping with the disease can feel overwhelming. However, many people go on to live fulfilling lives after treatment, and understanding what to expect can make the journey a bit easier.
Coping Strategies for Patients and Families
Dealing with the emotional and mental toll of oral cancer is just as important as managing the physical symptoms. It’s common to experience fear, anxiety, and uncertainty during treatment. Patients might worry about changes in their appearance, speech, and ability to eat or swallow.
Family members also play a key role in the recovery process. They can offer emotional support and help with day-to-day tasks, such as transportation to appointments or managing meals. Open and honest communication is important—talking about feelings, concerns, and fears can help reduce the burden on both the patient and their loved ones.
Rehabilitation: Speech Therapy and Reconstructive Surgery
After the treatments, the road to recovery can be long. Speech therapy often becomes a part of it. It helps those who struggle with speaking clearly due to the cancer or its treatment. For some, surgery to rebuild parts of the mouth or face is a must. Removing parts of the jaw, tongue, or face can leave scars, but surgery helps rebuild confidence and function.
With therapy and surgeries, patients can regain parts of their old lives. They can speak, eat, and laugh again. With patience, support, and hard work, the chance to return to normalcy grows.
Support Networks and Mental Health Help
The road doesn’t need to be walked alone. Support groups are lifelines. These groups, whether online or in person, give a place for people to share their stories. Others, in similar battles, can offer advice and comfort.
There are professionals ready to help with the mind and emotions. Cancer-focused therapists, counselors, and social workers guide patients and families through their emotional struggles. These experts can be a great help during tough times.
FAQs About Oral Cancer
1. Are there activities that increase the risk of oral cancer?
Yes, several habits can raise your risk, such as:
- Smoking cigarettes, cigars, or pipes.
- Using smokeless tobacco (chewing tobacco, snuff, or hookah).
- Excessive alcohol consumption.
- Prolonged sun exposure without lip protection.
- Having HPV (human papillomavirus).
- A family history of oral cancer.
Still, around 25% of cases occur in individuals with no clear risk factors.
2. What does oral cancer look like early on?
Early signs can include:
- White or red patches in the mouth.
- Non-healing sores.
- Lumps or thickened areas on the tongue, gums, or cheeks.
Regular dental visits and self-checks can help catch these early changes.
3. How is oral cancer treated?
Treatment often depends on the stage and location but may involve:
- Surgery to remove the affected tissue.
- Radiation therapy to destroy cancer cells.
- Chemotherapy to stop the growth of cancer cells. Emerging options like immunotherapy are also gaining traction.
Can oral cancer be prevented?
While not all cases are preventable, you can lower your risk by:
- Avoiding tobacco and excessive alcohol.
- Getting the HPV vaccine.
- Maintaining good oral hygiene and regular dental check-ups.
5. How does oral cancer differ from gum disease?
Gum disease stems from poor oral hygiene and causes inflammation, bleeding, or tooth loss. Oral cancer, on the other hand, involves abnormal cell growth that can spread and become life-threatening. Persistent sores or unusual patches should be examined by a professional.
6. Can you die from mouth cancer?
Yes, if left untreated, mouth cancer can be fatal. However, early detection significantly improves survival rates, making awareness and regular screenings essential.
Last Words
Oral cancer is a serious and often misunderstood disease, but it doesn’t have to be a death sentence. With early detection, treatment options have greatly improved, and many people go on to live healthy lives after their diagnosis. Awareness, regular check-ups, and understanding the risks and symptoms can help you protect yourself.
By keeping an eye on your health, avoiding known risk factors, and seeking medical attention when necessary, you can make a significant difference in the fight against oral cancer. Stay informed, stay proactive, and take care of your mouth—it might just save your life.